Beckwith-Wiedemann syndrome (BWS) is a genetic disorder causing overgrowth in babies and children. The congenital condition, affecting about one in 15,000 births, can be recognized at birth since the baby will be born with several features of BWS. However, some babies may only have a single feature of the condition, such as an enlarged limb called hemihypertrophy or hemihyperplasia.
Although some babies may inherit this condition from their parents, most of them have new genetic abnormalities causing BWS. Cancer surveillance in early childhood and appropriate treatment can help the baby grow without complications.
Read this post to know about the signs, causes, diagnosis, treatment, and outcomes of Beckwith-Wiedemann syndrome (BWS) in babies.
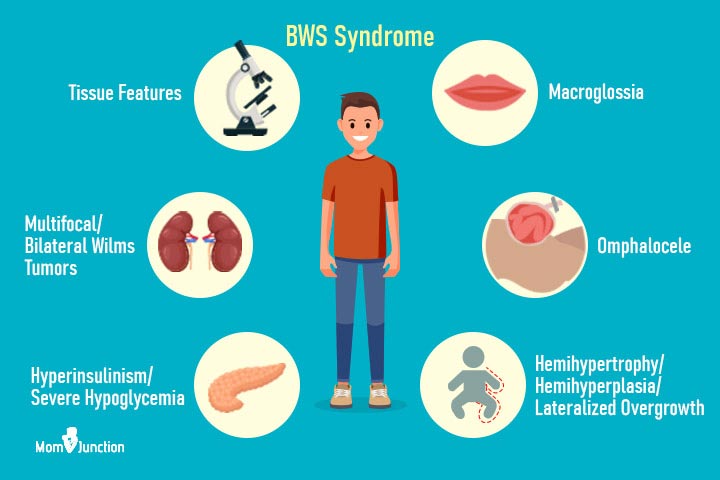
Signs And Symptoms Of BWS In Babies
The physical features of Beckwith-Wiedemann syndrome are part of the 11p overgrowth or 11p overgrowth spectrum. 11p overgrowth includes overgrowth and other features associated with genetic changes at the 11p region of chromosome 11. These features may include (1):
- Macrosomia is increased birth weight and length
- Hemihypertrophy or hemihyperplasia is an overgrowth of one side or part of the body
- Macroglossia is an enlarged tongue
- Hypoglycemia (low blood sugar) or prolonged hypoglycemia during the newborn period due to hyperinsulinism (increased insulin levels)
- Enlarged abdominal organs such as the liver, pancreas, and kidneys
- Abdominal wall defects such as omphalocele or umbilical hernia where abdominal organs protrude outside the abdominal cavity
- Creases and pits on the earlobe or behind the ear
Causes Of BWS In Babies
Several genetic factors are known to cause Beckwith-Wiedemann syndrome. Changes in gene expression of one or more genes on 11p15 regions on chromosome 11 can cause BWS. In some cases, BWS can be due to mutations of the CDKN1C gene on chromosome 11 (2).
BWS can be of two types depending on the cause (3).
- Sporadic Beckwith-Wiedemann syndrome and hemihypertrophy account for 85% of cases. These genetic changes occur sporadically without any inheritance. This can be due to improper inactivation of growth-suppressing genes or overexpression of genes encouraging growth. Sporadic BWS occurs without a family history, and there is no risk of having another child with the same condition.
- Inherited Beckwith-Wiedemann syndrome or isolated hemihypertrophy accounts for 10 to 15% of cases. Since it is hereditary, it is passed from parents to their children. There is a 50% chance of an affected parent passing this genetic abnormality to a child. Most hereditary cases are associated with CDKN1C mutation on chromosome 11. This condition can be passed to the next generation, and there is an increased risk of having another child with the syndrome.
The genetic changes may occur only in some cells, resulting in mosaicism. It means that some parts of the body have normal cells with normal gene expression on chromosome 11. This heterogeneity of gene expression is responsible for clinical features called 11p overgrowth.
Diagnosis Of BWS In Babies
BWS can be diagnosed clinically by observing the physical features. However, genetic testing is often ordered to confirm the diagnosis since this can explain the cause.
Babies with hemihypertrophy require evaluation from geneticists since this can also be seen as an isolated anomaly or with BWS. Blood samples or tissue samples are collected for genetic testing.
Cancer Risks And Screening In BWS
Babies with Beckwith-Wiedemann syndrome and isolated hemihypertrophy may have an increased risk of developing certain childhood cancers. Approximately 5-10 percent cancer risk is estimated in children with BWS, but this may vary depending on the cause of BWS (3).
The following cancers are often associated with BWS in babies (3).
- Wilms tumor is kidney cancer, most commonly seen in BWS. Nearly 95% of Wilms tumors occur in babies with BWS before age seven.
- Hepatoblastoma is liver cancer and the second most common type of cancer associated with BWS or isolated hemihypertrophy. This cancer is usually present by two years of age.
- Other rare childhood cancers such as neuroblastoma (affect nerve cells), rhabdomyosarcoma (involves soft tissue such as skeletal muscle tissue), and adrenocortical carcinoma (affects the outer layer of adrenal glands) can also be associated with BWS.
Regular screening is recommended for babies with BWS until teenage to detect cancers as early as possible. The prognosis depends on the cancer spread since early detection and treatment can improve outcomes. Early detection may also reduce the need for chemotherapy and radiotherapy or may require low-dose therapies.
The following screening tests are usually recommended for babies with BWS.
- Abdominal ultrasound every three months until seven years of age. Images of the liver, kidneys, and other abdominal organs are obtained until four years since the risk for liver cancer declines beyond this age. The renal and adrenal glands ultrasound is obtained until seven years of age.
- Alpha-fetoprotein (AFP) levels in the blood are screened every three months until four years of age. This protein is released by immature or damaged liver cells, and higher levels indicate a risk of hepatoblastoma. AFP can be normally high in the newborn period, and it may decline later.
Babies with clinical features of BWS and negative genetic test results may also receive similar cancer surveillance and medical management as babies with positive genetic tests results.
Treatment For BWS In Babies
There is no cure for BWS in babies. The existing measures focus on treating symptoms and surgical correction of physical features. The following treatments are given according to the physical features of BWS in babies (4).
- Abdominal wall repair for umbilical hernia is usually done soon after birth.
- Hypoglycemia treatment and monitoring of glucose levels every six hours is done for the first few days of life.
- Pancreatectomy (surgical removal of the pancreas) may be considered if there is severe hypoglycemia.
- Maxillofacial surgery may be required to treat macroglossia. Speech-language therapists may be involved in the care of macroglossia since this may often cause feeding and speech difficulties and drooling.
- Orthopedic surgeries to correct the leg lengths are done in later years if one leg is larger than the other. Special orthopedic shoes with adjusted heels are recommended until surgical repairs.
Doctors may give future follow-up plans with various medical specialists such as endocrinologists, orthopedists, plastic surgeons, and oncologists to evaluate and treat possible complications of BWS.
Outlook Of BWS
Most babies with BWS and isolated hemihypertrophy may grow up normally. Physical features may become less noticeable when the child grows and could often be corrected with subsequent surgeries. They may appear larger than their peers in early childhood, but their growth declines gradually.
Most babies with BWS tend to have normal growth and reduced cancer risk by adolescence. Most grow up to be adults with above-average height and normal intelligence and lifespan. BWS does not interfere with reproduction in the future.
BWS in babies may require long-term follow-up care as recommended by the healthcare provider. Adequate care helps to identify and treat cancers in the early stages. Genetic counseling helps the parents understand the chances of having a second child with BWS. You may ask the pediatrician to know better healthcare plans and programs to facilitate and finance the various treatments required for BWS care.